Hyperoside ameliorates the injury of heart and thoracic aorta in mice with myocardial infarction by regulating autophagy pathway
YANG Yongkang, LI Jing, RAO Tingcai, ZHANG Junyan
2021, 26(6):
601-608.
doi:10.12092/j.issn.1009-2501.2021.06.001
 Asbtract
(
506 )
Asbtract
(
506 )
 PDF (14971KB)
(
165
)
Related Articles |
Metrics
PDF (14971KB)
(
165
)
Related Articles |
Metrics
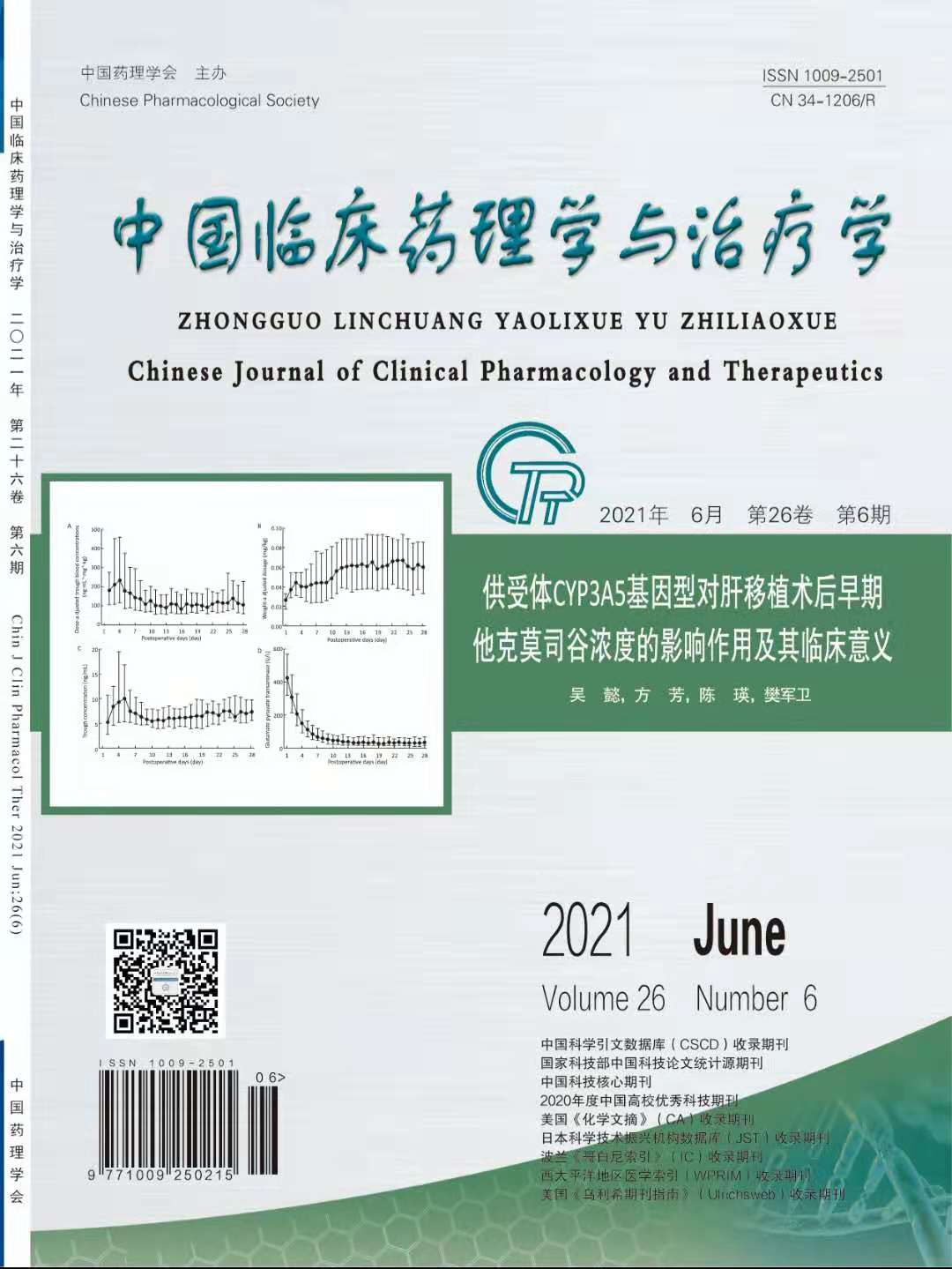
AIM: To explore the protection of Hyperoside (Hyp) on heart and thoracic aorta in mice with myocardial infarction (MI) as well as its potential mechanism. METHODS: The MI model was generated by a ligation on the left anterior descending coronary artery. The mice were then randomly divided into sham group (saline, 0.1 mg/10 g), model group (saline, 0.1 mg/10 g), Hyp-low, moderate and high concentration groups (Hyp, 9, 18 and 36 mg/kg), Fosinopril group (Fosinopril, 15 mg/kg), and Hyp-high concentration + 3-MA group (Hyp, 36 mg/kg; 3-MA, 30 mg/kg). The mice were treated with Hyp and Fosinopril for two weeks, and then the changes of heart weight versus body weight (HW/BW), electrocardiogram (ECG) remodeling, cardiac function, oxidative stress level in serum, thoracic aorta remodeling and endothelial function were investigated. RESULTS: In the model group, the HW/BW was elevated (P<0.01). The width of QRS in ECG was elevated, as a company with the reduction of height of QRS (P<0.01). The echocardiography assay showed that the cardiac cavity was enlarged (P<0.01). The oxidative stress level in serum was enhanced (P<0.01). The thoracic aorta remodeling and endothelial dysfunction became more serious (P<0.01). After being treated with different concentrations of Hyp and fosinopril for two weeks, the changes above were reserved (P<0.05, P<0.01). Co-treatment with 3-MA, an autophagy inhibitor, suppressed the protective effects of Hyp on impaired hearts and vessels (P<0.05, P<0.01). CONCLUSION: Hyp has protective prospects on injured heart and thoracic aorta remodeling, as well as endothelial dysfunction in MI mice; 3-MA, an autophagy inhibitor, can reverse the cardiovascular protection of Hyp. The mechanism may be explained that Hyp can elevate autophagy level in heart, which further weaken oxidative injury in MI mice.